Medicare Part D – CMS Notification Reminder!
Employers with group health plans, regardless of type, must report the “creditable” status of their prescription drug coverage to CMS. This means informing them if the plan meets Medicare standards for cost and coverage. Employers do this through an online portal and must report:
- Annually: within 60 days of the plan year starting.
- Termination: within 30 days of the plan ending.
- Changes: within 30 days of any status change.
For example, a calendar year plan (January-December) reports by February 29th. Additional resources including reporting guides are available at CMS’s online reporting system.
1095‑B Forms for Fixed Funding Groups Under 50 Lives
Fixed Funding groups under 50 lives will receive pre-completed 1095-B forms from AmeriHealth Administrators in late January, mailed (this letter) and emailed to contacts and brokers. Birthdates replace social security numbers on the forms, as allowed by the IRS.
Humira Replaced by Biosimilars in Major Formularies Starting April 1st
CVS Caremark and Aetna are making changes to their formularies to promote the use of biosimilars, similar to generic drugs but for biologic medications. This aims to lower specialty drug costs, particularly for Humira, which will be removed from many formularies as of April 1st.
These biosimilars are safe, effective, and offer cost savings of up to 27% for autoimmune treatments. CVS Caremark and Aetna assure smooth transitions for both doctors and patients through digital tools and support resources. They highlight a historical adoption rate of 94% for biosimilars in similar situations.
Overall, this change emphasizes cost savings and ease of transition for biosimilar adoption, offering significant cost benefits for plan sponsors and affordability for members.
New Jersey Enacts Infertility Coverage Mandate
New Jersey mandates fully insured large group plans and state and school employees
to cover infertility and related services starting August 1st, 2024. This applies to:
- Large group fully insured plans with pregnancy benefits.
- State and School Employees Health Benefits Programs.
Covered services include IVF, insemination, genetic testing, and more. Notably:
- Partner coverage after successful sterilization reversal is included.
- Denials based on relationship, sexual orientation, and age are prohibited.
- Age-based restrictions on coverage are absent.
Utilization reviews based on medical necessity are allowed, following ASRM guidelines.
Religious employers can opt out of covering specific procedures if it conflicts with their beliefs. Overall, this law expands access to crucial infertility treatments for many New Jersey residents.
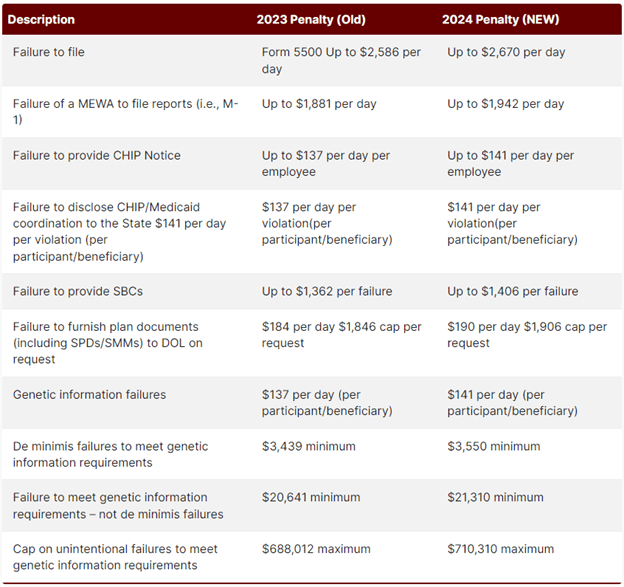
Compliance Corner! DOL Penalties Increase for 2024
The Department of Labor has increased penalties for certain employee benefit plan violations in 2024, including:
- Missing required notices
- Late Form 5500 filing
- Unresponsive to document requests
Overall, it’s crucial for employers to be diligent in complying with benefit plan requirements and responding to EBSA requests to avoid costly penalties.

Rob is an employee benefits expert with over 25 years of experience. He is the founder and principal of Precision Benefits Group, a leading provider of corporate benefits plans. He is a member of the Philadelphia Business Journal Leadership Trust and regularly contributes to the publication.
